PTAB with DETOUR System: A New Treatment Option for Patients with Complex Peripheral Artery Disease (PAD) Now Available
Arizona Endovascular Center Arizona Endovascular Center • March 25, 2024
PTAB with DETOUR System
Arizona EndsoVascular Center is committed to providing patients with the latest and most innovative treatments for Peripheral Arterial Disease (PAD). We are excited to announce that we now offer Percutaneous Transmural Arterial Bypass (PTAB) using the DETOUR System, an innovative percutaneous therapy designed specifically for long complex femoropopliteal disease.
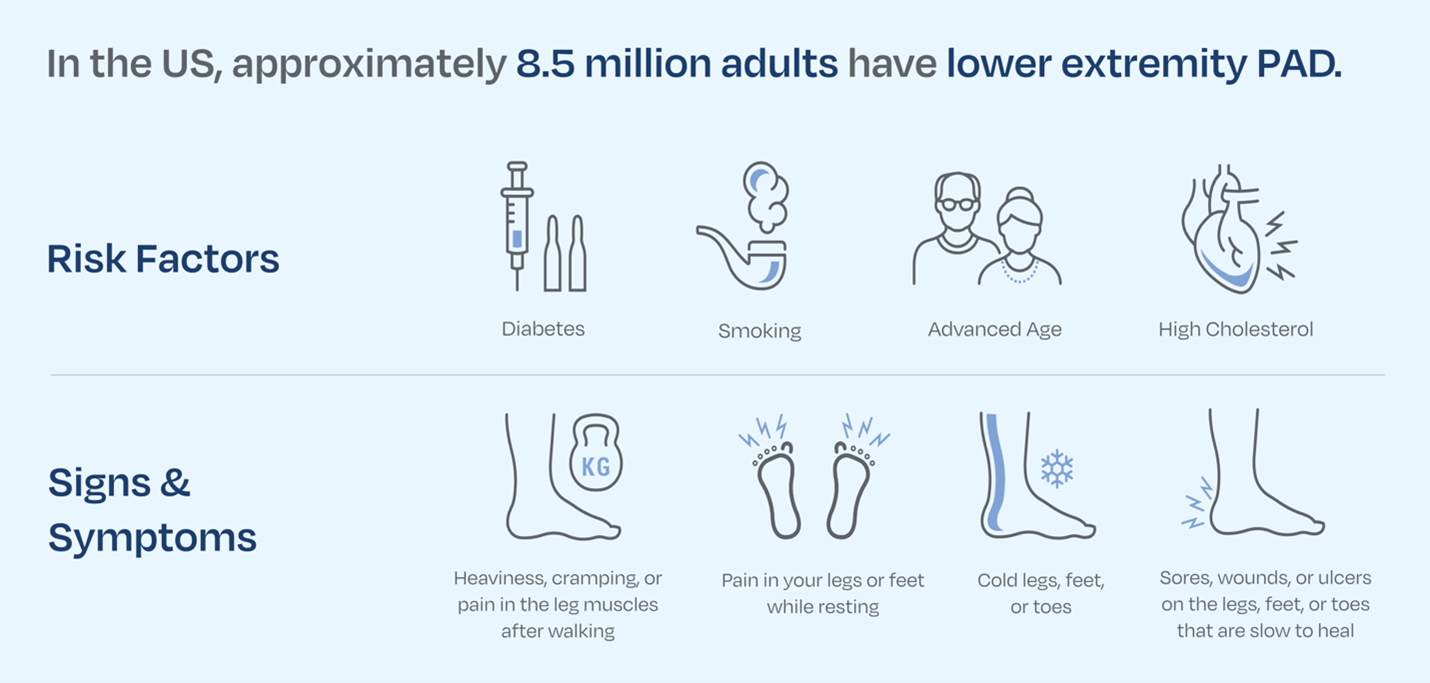
PAD is a circulatory problem caused by blockages in the arteries, which can lead to a reduction in the flow of oxygenated blood to your body, particularly in your lower limbs. If left untreated, PAD can cause pain, loss of mobility, sores on your legs, feet or toes, and in severe cases, amputation.
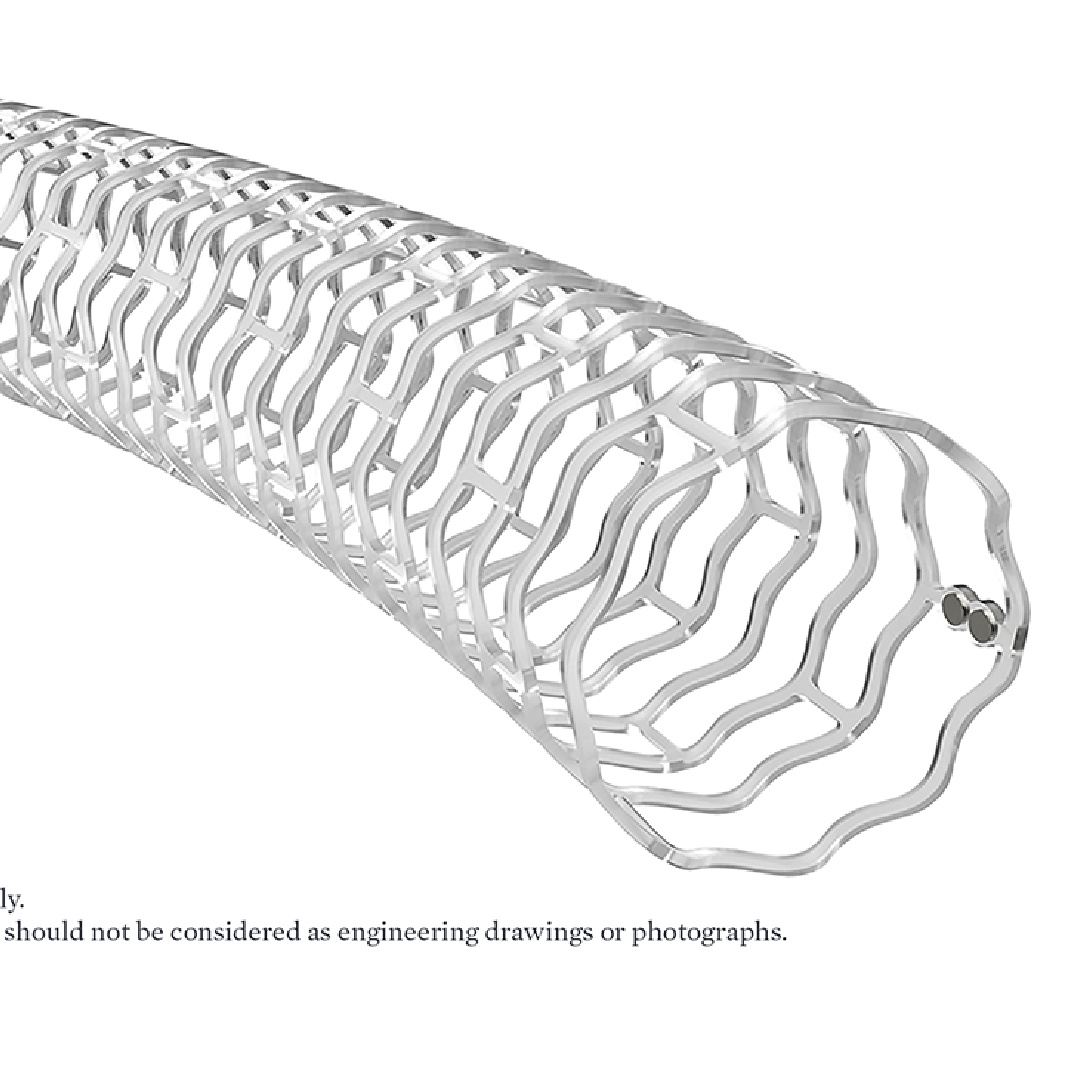
PTAB with the DETOUR System provides an innovative alternative option that is minimally invasive and offers fast recovery times. PTAB with the DETOUR System is a minimally invasive approach that utilizes endovascular techniques and the patient’s own vasculature to create a bypass around the diseased area.
During the PTAB, your doctor will implant stent grafts that will pass through the arterial wall, into the adjacent vein, and back into the artery. The bypass created with the stent grafts will re-direct blood around the blockage to increase flow.
Our team of experienced physicians
and healthcare professionals is dedicated to delivering the highest quality patient care and providing our patients with the best possible outcomes.
For more information about PTAB using the DETOUR System and if you’re a candidate for this therapy, call us to schedule a consultation
so that you may talk to your doctor to review the risks and benefits of this therapy.
Data source
AHA Statistical Update. Heart Disease and Stroke Statistics—2022 Update: Summary. Circulation.2022;
145:e153–e639. DOI: 10.1161/CIR.0000000000001052

Leg swelling and pain can be caused by a variety of factors, but when should you consider it a potential sign of a blood clot? Understanding the warning signs can help you take timely action. Signs That Your Leg Swelling Might Be Due to a Blood Clot: Swelling that occurs suddenly and is localized to one leg Pain that feels like cramping or soreness Skin that appears red or feels warm to the touch When to Seek Medical Help : If you experience persistent swelling, pain, or any of the above symptoms, it’s essential to seek medical evaluation promptly. Untreated blood clots can lead to serious complications such as pulmonary embolism. What to Expect During Evaluation: Physical examination Ultrasound imaging to detect clot presence Blood tests to assess clotting risk Arizona Endovascular Center offers expert diagnosis and minimally invasive treatments to address blood clots and ensure optimal vascular health.
Preventing blood clots is essential for maintaining good vascular health and avoiding complications such as DVT and PE. Fortunately, there are simple lifestyle changes you can adopt to lower your risk. Stay Active: Regular movement helps keep blood flowing and prevents clot formation. If you have a sedentary job, take breaks to stretch and walk. Maintain a Healthy Diet : Incorporate foods rich in omega-3 fatty acids, fiber, and antioxidants to support circulation and overall heart health. Stay Hydrated: Proper hydration helps maintain optimal blood viscosity and reduces the risk of clot formation. Know Your Risk Factors: If you have a history of DVT, are pregnant, or have underlying health conditions, consult with a specialist to develop a personalized prevention plan. Arizona Endovascular Center is here to help you take proactive steps to reduce your risk of blood clots and improve your vascular health.

At Arizona EndoVascular Center, we believe that the heart and blood vessels are intricately connected, with one’s vascular health directly impacting heart health. Understanding the vital relationship between these systems is essential to maintaining overall well-being. The circulatory system comprises the heart, arteries, veins, and capillaries. When your blood vessels are compromised by conditions such as atherosclerosis (plaque buildup), varicose veins , or other vascular diseases, the heart works harder to circulate blood throughout the body. Over time, this can lead to heart failure, strokes, or heart attacks. Key factors that affect both heart and vascular health include high blood pressure, smoking, poor diet, lack of exercise, and diabetes. These risk factors can damage blood vessels, leading to an increased risk of cardiovascular diseases. Taking proactive steps to maintain your vascular health through regular exercise, a balanced diet, and routine checkups can help prevent complications and promote heart health. Regular screenings at Arizona EndoVascular Center can catch early signs of vascular issues before they worsen, ensuring that both your heart and vascular systems stay in top condition.

As the temperatures drop, those with varicose veins may notice an increase in discomfort. Cold weather can exacerbate symptoms, but there are steps you can take to manage varicose veins and reduce symptoms. Here’s how to manage varicose veins during colder months: Layer Up – While staying warm is important, be mindful of wearing tight clothing that can restrict blood flow. Opt for loose, comfortable layers that allow circulation to move freely. Keep Moving – Cold weather can make people want to stay indoors, but regular movement is crucial for promoting good circulation. Aim for gentle exercises like walking or stretching to keep blood flowing to your legs. Use Compression Stockings – These special stockings provide gentle pressure to support the veins and improve circulation, helping to reduce swelling and discomfort in cold weather. Moisturize – Cold, dry air can irritate the skin around your veins. Regularly moisturizing your skin can reduce dryness and improve comfort. Elevate Your Legs – If you’re spending time inside, take breaks to elevate your legs above your heart to reduce swelling and promote better circulation. If cold weather is causing significant discomfort, don’t hesitate to reach out to Arizona EndoVascular Center for advice on more advanced treatment options to alleviate symptoms.
Arizona Endovascular Center, led by Dr. Sara McKeever, proudly announces the successful implantation of Abbott’s Esprit™ BTK Everolimus Eluting Resorbable Scaffold System (Esprit™ BTK System) , a groundbreaking dissolvable stent designed for patients suffering from chronic limb-threatening ischemia (CLTI) below-the-knee (BTK). Approved by the U.S. Food and Drug Administration (FDA) in April 2024, the Esprit BTK System offers new hope for individuals facing the most severe form of peripheral artery disease (PAD). The Esprit BTK System is an innovative bioresorbable scaffold designed to support the artery during the critical healing process. It delivers the drug everolimus to aid vessel healing before gradually dissolving, leaving behind a naturally functioning artery. Composed of materials similar to dissolving sutures, the scaffold is implanted through a minimally invasive, catheter-based procedure. It provides crucial support to the artery until it can maintain its own structural integrity. “The FDA’s approval of the Esprit BTK System represents a significant advancement in below-the-knee therapy,” said Dr. Sara McKeever . “This new treatment option not only supports healing but also reduces the risk of long-term complications. We are excited to offer our patients the latest technological innovations to address chronic limb-threatening ischemia and improve their quality of life.” Chronic limb-threatening ischemia (CLTI) is a severe form of PAD that occurs when arteries become obstructed with plaque, preventing adequate blood flow and oxygen from reaching the lower leg and foot. PAD affects over 20 million people in the U.S., yet only 10% of cases are diagnosed. The disease disproportionately impacts Black and Hispanic communities, with nearly 1 in 3 Black adults and 1 in 5 Hispanic adults developing PAD. Arizona Endovascular Center remains committed to pioneering advanced treatments for PAD and improving patient outcomes with state-of-the-art technology like the Esprit BTK System.







